 I am very privileged to be on this US ‘person-centred’ study tour (see prelude & part 1 of tour here) with a clinician who has worked half their life in Australia and half in Georgia, USA. They currently work in the US and have joined me on this tour which is both enlightening and also opening many extra doors, enabling detailed insights into US systems and the impact of recent large-scale patient-centred healthcare reforms.
I am very privileged to be on this US ‘person-centred’ study tour (see prelude & part 1 of tour here) with a clinician who has worked half their life in Australia and half in Georgia, USA. They currently work in the US and have joined me on this tour which is both enlightening and also opening many extra doors, enabling detailed insights into US systems and the impact of recent large-scale patient-centred healthcare reforms.
Family and friends in the US have also very kindly made some medical appointments while I am visiting so I can accompany them and experience medical visits from a patient perspective. Call me a secret shopper but this is providing the most amazing opportunity to access a variety of healthcare environments that as a foreigner I would not normally be able to access. Where I have not been able to have a ‘patient’ appointment, my local contacts have been able to secure an informal tour on various occasions.
Staff we have interviewed during our visits to US healthcare facilities:
- Orthopaedic Specialist
- Cardiologist
- Primary Care Physician
- 2 Physician’s Assistants
- 2 Nurse Practitioners
- 3 Licensed Practical Nurses
- 3 Registered Nurses (including Nurse Manager for ICU & PCU at acute care hospital)
- 2 Occupational Therapists
- 1 Occupational Therapy assistant
- Speech Pathologist
- Physical Therapist
- 2 Medical Practice Assistants
- 2 Directors of Rehab
- 2 Office Managers
This study tour has included a paediatric outpatient clinic, a skilled nursing facility (nursing home residents and sub-acute rehabilitation), an acute care hospital, a specialised cancer treatment hospital, a HMO (Health Maintenance Organisation) with 2 specialist appointments – orthopaedic and cardiology, an urgent care/primary care physician and a 66 bed sub-acute rehabilitation facility.
Study Tour Part 2: Georgia
- Gordon Hospital, North West Georgia
- Infinity Children’s Services: OT, Physio & Speech Therapist, Calhoun
- Rehab Centre & Aged Care Facility, North Georgia
- Walmart Pharmacy, North Georgia
Atlanta:
- Cardiologist appointment including ECG – Kaiser Permanente Specialist clinic
- Orthopaedic procedure – cortisone injections in both knees – Kaiser Permanente
- Specialist clinic
- Kaiser Permanente Flu clinic
- Kaiser Permanente Pharmacy
- Cancer Treatment Centre of America – 1.5 hour tour of facility
- Rehab centre
- Aged Care
- CVS Pharmacy
Take a tour with me:
Hospital & Paediatric Allied Health Care Facilities, North Georgia
Allied Health, Rehab and Aged Care facilities, Atlanta,
Cancer Treatment Center of America, Atlanta
Cardiology visit and Orthopaedic procedure, Atlanta
Visit 2: Cardiology Consultation & ECG, Kaiser Permanente, Atlanta, Georgia, USA
Patient Scenario:
Ron is about to turn 65 and has become concerned about his heart health after two of his younger and seemingly healthier work colleagues died suddenly from heart attacks. Ron realises he is at high risk having diabetes, asthma, high blood pressure, a stressful job and being overweight.
 Step One: Appointment & booking process:
Step One: Appointment & booking process:
Ron’s insurance is with Kaiser Permanente. While Ron has a patient portal (referred to as “KP.org”) which he knows he can use to make appointments, he prefers to call to make appointments. Time-management is his priority so he made appointments to visit both the Cardiologist and the Orthopaedist on the same day. Because Ron’s insurance is with Kaiser he only sees Kaiser doctors. There is a centralised booking system and the Specialists are located in the same premises. At each point of contact Ron’s details were verified with name, DOB, address, telephone number and the Kaiser Medical Record Number (MRN). Many patient jokes are made about the importance of the insurance card.
Cost & Insurance
Ron had a choice of insurers when commencing employment and chose Kaiser Permanente insurance. If you are with Kaiser Permanente you need to attend ‘a Kaiser clinic’ or a hospital that accepts Kaiser insurance. Kaiser, Georgia has 555 Physicians representing all specialities. They have 3,694 staff and 364,164 members.
Kaiser have a very proactive approach to preventive health and encourage regular health checks and screening. They proactively identify care gaps and have a reward system designed to incentivise patients to attend regular check-ups and/or to engage with health coaches.
Ron was advised there would be a total $80 copay for the two specialist consultations, $40 each visit.
Step Two: Checking In
Ron had attended this large facility before so proceeded straight to a clearly marked ‘Check In’ area. There were large signs directing patients to electronic check-in kiosks however Ron said he prefers to speak to people. There was a queue of about 5 patients and while in the queue a staff member was approaching patients and gently asking if they would like help learning how to electronically check in. I was informed the self check-in kiosks were new.
The receptionist then verified Ron’s details and confirmed he was attending two specialist visits. Payment of $80 was taken at check-in for the two Specialist ‘co-pays’. There was a little bit of stress as patients are aware they need to attend 15 minutes before their appointment to complete check-in processes and update any demographic information. They know that if they are late there will be a fee charged. It was vital also to Ron that his first appointment run to time as the two specialist appointments were scheduled only half an hour apart. While Ron was advised to return to the check-in desk after his cardiology appointment, the receptionist reassured Ron all departments could see (via their Epic software system) that Ron was in the facility and at what stage of his visits he was up to and they would run to time.
Step Three: Consultations
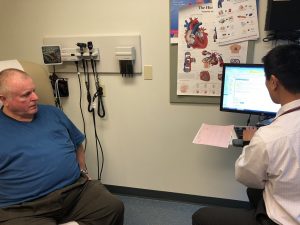
On arrival Ron was taken to a consulting room where he remained for the duration of the half hour visit. During this time 3 clinicians came into the room:
Clinician 1: A Licensed Practical Nurse (LPN) confirmed Ron’s details in his electronic medical record (EMR) including checking item by item through his medication list, medical history and allergies. As the LPN checked each item she ticked to notate that it had been checked. She then took Ron’s ‘vitals’ (writing measurements on paper) and performed an ECG. The LPN then entered all observations into the EMR (Epic) while conversing with Ron.
Clinician 2: The Cardiologist then arrived and it was clear he had already checked the electronic medical record. He went through the medical history and medication lists (even though the LPN had done the same) and Ron then mentioned he had never taken one of the listed medications. The Cardiologist had a general chat with Ron, updated details in the EMR, discussed ECG results and then had a lengthy conversation regarding options for further testing and treatment. The doctor and Ron spent quite a bit of time negotiating a treatment plan they were both happy with. The Cardiologist typed his notes directly across from Ron while verbalising exactly what he was writing to confirm the decisions they had made together. He also advised he would print out the action plan and that Ron could also access the plan, his results and his entire medical record himself at any time (through kp.org). He left the room advising that his assistant would soon be in to help Ron.
Clinician 3: A Medical Assistant (MA) came into the room within 1 minute. There would not have been time for a verbal handover from Cardiologist to MA so he must have read the EMR as he was completely up to speed as he verbally summarised to Ron what had taken place so far in the consultations. He told Ron he was going to now generate the request for the stress test and he also printed some recommendations for Ron as well as the ‘Discharge Summary notes’ from the visit. Ron was asked if he had any questions or any information that needed clarifying. When Ron said he didn’t he was then informed that he could email or call with questions at any time.
Clinician 4: Ron moved downstairs to level one of the same building, to Pharmacy. Here he joined the ‘check-in’ queue. A Pharmacy Assistant verified his details including his medication history and instructions received from the Cardiologist via the EMR. Ron asked a question about his medication and was advised he would check with the Pharmacist and was told to take a seat and wait to see his name on the board for the check-out.
Clinician 5: From the check-out area the Pharmacist called Ron’s name and clarified the change in medication. He also answered all Ron’s questions, provided medication education and reassurance.
Patient Ron’s Comments
- “First time I’ve seen that Cardiologist; I really liked him, he really listened. I was really impressed when I told him I didn’t have a Cardiologist and he said “you do now, you have me”.
- “He was real nice about you being in the room.”
- “That MA was an army corpsman, they are frontline medics. Everyone in these places are so good.”
- “Sometimes it feels odd that you are left alone in the room. Not today but other times I have waited alone in there for 30 minutes. When that happens I worry they have forgotten me.”
Clinician Comments
- “That was a great example of a challenging patient presentation and impressive patient communication skills; he really does need that stress test”.
- “Having a nurse at a desk in the waiting room just in case someone wants a flu shot seems over the top. America seems obsessed about the flu vax.”
- “I think it’s a safety risk that patients are left alone waiting for the clinicians to come in to them.”
My Practice Management & Health IT Assessment:
- Very impressive, efficient large scale multidisciplinary healthcare facility.
- Protocol driven approach with every staffmember seemingly clear on their scope of practice for each particular role.
- It was a challenging consultation for many reasons and the cardiologist was fantastic. He had a wonderful patient-centric approach in identifying what is important to the patient in order to successfully negotiate clinical goals and commitment to an action plan.
- The co-ordinated team approach between Assistants, Nurses and Doctors seems to work well. Everyone seemed to know their roles and timing. They clearly write detailed, effective notes for each other and are very dependant on quickly reading these notes to ensure they are up to speed for each patient.
- I did not initially see the point in having an MA attend after the Cardiologist as the doctor was clearly more than capable of generating the stress test request however it provided another opportunity for the patient to ask questions. The MA was very experienced however the Specialist was still located outside in the department if there were questions that needed clarification.
- Ron was encouraged to use health information and electronic education tools to further build understanding of his own conditions and risk management.
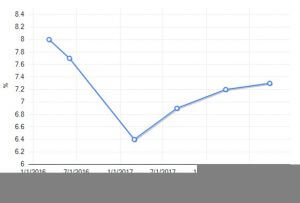
- Graphs of Ron’s previous results in his EMR were used as an education and motivation tool and Ron was encouraged to access his own results (particularly in relation to his diabetes) via the patient portal (kp.org) and track improvements.
I will be writing up all my visit reports from Georgia on my return so let me know if you are interested in reading more or learning about any specific aspects of healthcare delivery in these centres.
Slight details and names have been changed to protect privacy but a huge thank you to patient Ron for so generously allowing me the privilege of sharing a day in his health journey.
Next stop New York…

