Health Care Homes – Blog 1 of 4 part series
What Practice Managers need to know:
- The way we provide healthcare in Australia is changing.
- Differing models are being trialled.
- Practices that evolve and adapt will be the ones who survive.
Some of the reasons major change is needed:
- Our patients are living longer with complex health needs.
- Medicare in its current form is unsustainable.
- Prevention, continuity of care and improved co-ordination is vital for health improvement.
- Patient expectations are changing.
- New technologies are transforming the way we can work.
Design your own improvements
Imagine if doctors had time to talk to patients on the phone or via a quick telehealth consultation?
Imagine if patient-care decisions didn’t all involve whether we could bill Medicare?
Imagine if we could make life easier for patients by… [insert your team’s wishlist]
Imagine if we could make our clinicians happier by… [insert your team’s wishlist]
Now is the time to think creatively. What innovations would you like to try?
Alternative models of care are being officially & unofficially ‘trialled’
Health Care Home (HCH) official trials are taking place in Australia right now. Read more about Dept of Health official ‘Health Care Home’ trials
‘Readiness’ programs – with varying names like Patient Centred Medical Neighbourhood, Patient Centred Collaborative Care, Comprehensive Primary Care etc – are currently supported by many Primary Health Networks. These ‘readiness’ sites have most of the fundamental changes of a health care home without trialling a new funding model.
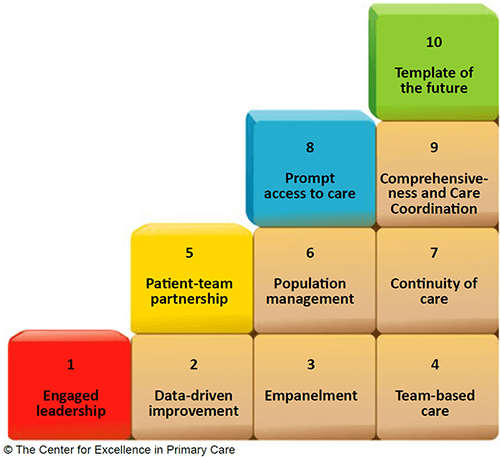
Like Health Care Homes they are focused on putting in place all the ‘building blocks of high-performing practices’ and exploring alternative and innovative ways to provide patient-centred care.
The 10 Building Blocks of ‘high performing’ practices
Bodenheimer T, Ghorob A, Willard-Grace R et al. The 10 building blocks of high-performing primary care. Annals of Family Medicine 2014; 12(2):166-171.
The official Health Care Home sites are also trialling a new funding model, where patients are categorised according to their complex chronic condition needs and the practice receives funding per patient.
The practice then does not bill Medicare at all for visits which relate to the patient’s chronic conditions. Read AAPM Activity Monitoring Guide.
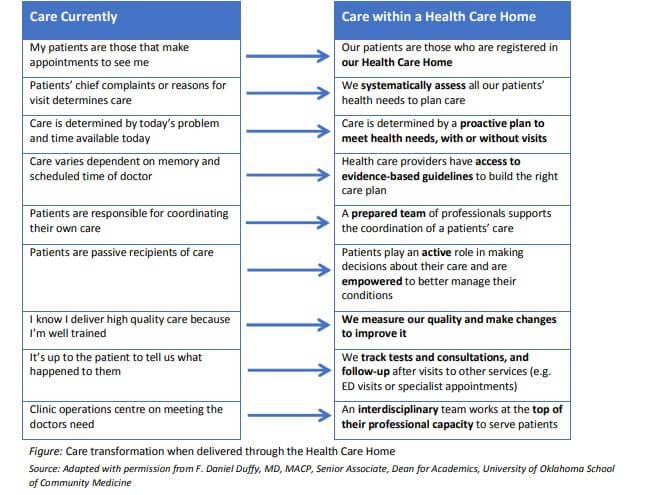
How different is all this from what we do now?
Data Driven Quality Improvements
Without accurate coded data, practices cannot easily identify co-morbidities (essential for allocation of funds), patients at risk nor track improvements in care, financial or health outcomes. In 2018 I have been working with many of the practices across Australia involved in these trials and readiness programs with a focus on data-driven improvements, change management and system improvements. Download a pdf of my presentation ‘Leading your practice into a digital future’.
What are the some of the major changes:
- Patients are ‘registered’ with your practice (continuity of care). In the official trials the ‘Health Care Home’ receives funding to manage ‘registered’ patients.
- Co-ordinators proactively assist patients. A new admin/assistant nurse role and qualification (Medical Practice Assistant) has emerged. Patients have a ‘care team’.
- Every aspect of care delivery – from uploading a shared health summary to a telephone call, has a $ amount allocated and is tracked.
- Electronic communication tools are used routinely – My Health Record and a shared care planning tool are used to improve communication and co-ordination of care.
5 things you can do right now:
- Build your practice ‘team culture’.
- Look for ways to engage your patients so they feel like they are ‘registered’ with your practice
- Improve your data quality.
- Look at what you are currently doing well and identify areas for improvement (encourage creative thinking). Measure your ‘quality improvements’ (doing this will put you in a good position to meet the new Standards for General Practices (5th edition) as well as impending Quality Improvement PIP changes too).
- Learn from other ‘high-performing’ practices.
I’d also suggest reading RACGP’s ‘Standards for Patient-Centred Medical Homes’ which align with the 5 elements of the ‘medical home’: 1. Patient-centred 2. comprehensive 3. co-ordinated 4. accessible and 5. quality care.
The only constant is change. We either keep up now or catch up later!
In Part 2 of this blog series next week I will report on some of the success stories as well as the challenges being reported from both official trial & readiness sites. The Train IT Medical team are also studying and will be reporting on alternative models of care (both onsite and online models) being set-up independently by clinicians keen to be at the leading edge of healthcare reforms. l am also doing a 3 week study tour of the US in October – you can follow my trip and learnings in future blogs or follow me on facebook or twitter.
I’d love to showcase your innovative practice! Send me your success stories and improvement ideas [email protected]
We all benefit when we share ideas and work together towards improvements in health care delivery.
Remember, every improvement came from change!
With best wishes, Katrina Otto
More free learning resources related to Health Care Homes are here.
Disclaimer: Please note I am an independent trainer and Practice Management Consultant. While I am an approved trainer for the Dept of Health, Australian Digital Health Agency, Primary Health Networks, AHPRA, AAPM, APNA, AHPA, MedicalDirector, Best Practice Software, Avant Mutual Group, MDA National etc and regularly present education sessions on behalf of organisations, the feedback and opinions expressed in these blogs are my own. Katrina Otto