This is the third in our blog series focusing on effective use of practice software to improve recall and reminder systems. At Train IT Medical we work with many practices and see successful recall and reminder systems however we also see a lot of frustration (unnecessary money wasted, time spent and stress) so we are keen to help all MedicalDirector Clinical software users maximise efficiency. Here are our top 5 tips:
Tip 1 – Differentiate between ‘Clinically Significant’ Recalls and ‘Preventive Health’ Reminders
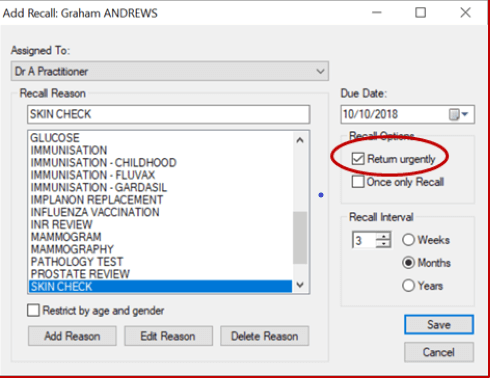
Within MedicalDirector’s Recalls feature there is a tickbox labelled ‘Return Urgently’ and it is this button that enables us to distinguish between recalls and reminders. For example, a ‘reminder’ for an annual skin check that is preventative in nature, and where there has been no previous abnormality, is completely different to a recall for a skin check for a patient previously treated for melanoma. A routine 5 year cervical screening test ‘reminder’ compared to a cervical screening test for a patient who has had previous abnormality. When indicated these ‘Clinically Significant’ recalls must be followed up until the patient returns or the doctor has said the patient no longer needs follow-up. To help identify these clinically significant ‘Recalls’ we can tick the box marked ‘Return Urgently’ (you might find it helpful to think of it as ‘Priority/Clinically Significant’ rather than ‘urgent’). We certainly don’t want to stalk our patients about their annual flu vaccinations or routine skin checks so managing these differently is essential to save time, money and also for patient/practice relationships.
Tip 2 – Control your Recall List
Essential to the success of any practice ‘Recall and Reminder System’ is a well-defined and controlled practice list – read Blog 1 ‘Recalls & Reminders, why is it so hard‘. We find successful practices have a recall and reminder list with no more than 30 reasons. They also contain generalised descriptions eg. ‘Blood Test’ or ‘Skin Check’, rather than dozens of reasons detailing every test or every body part.
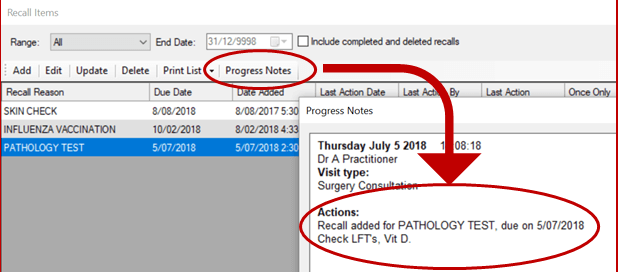
Important to the success of this is knowing you can see relevant detail if you click on the Progress Notes button from within the Recall Items window. The progress note from the day the recall was added will display, allowing easy identification (depending on quality of doctors’ notes) of why the recall was first created and what the doctor was planning when originally adding the recall to the patient file (especially helpful if the patient sees another doctor in the practice).
It is important for doctors to be told that when they add a recall from the Holding File (when actioning incoming correspondence), the recall reason defaults to the subject line on the highlighted item. For example, if a recall in response to a result with a subject line eg ‘E/LFT’, the default recall reason will have this same reason, regardless of whether it exists in your recall reason list in MD. It’s a good idea to make doctors aware of this as they may be unintentionally adding dozens of very specific reasons to the list. Whatever the ‘reason’ label says is what the patient will read so we need a well-defined practice list.
Tip 3 – Adopt a paperless approach to follow-up
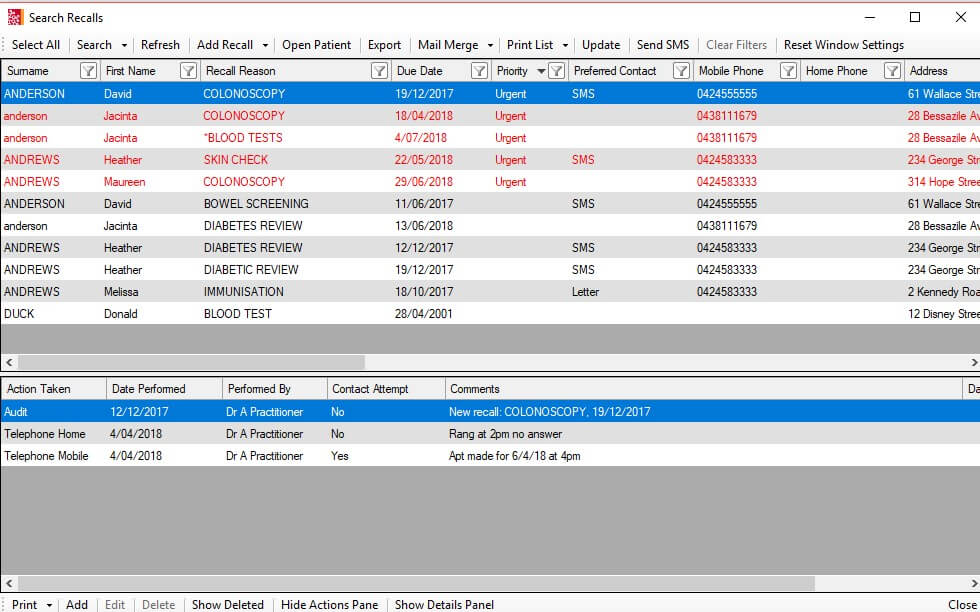
In more recent versions of MedicalDirector Clinical major improvements have been made to the Recalls functionality to enable us to be completely paperless. A well defined and managed list should enable both easy differentiation of Recalls versus Reminders as well as a clear audit trail of patient contact related to the recall. Remember there is no magic number when it comes to contact attempts – clarity within your practice system is vital.
Tip 4 – Record ‘Preferred Contact’
In the patient demographics section of MedicalDirector Clinical, collect informed consent for recall contact and notate ‘Preferred Contact’ eg SMS, as this will enable easily filtering and bulk sms messages (or mailmerged letters) to be generated.
Tip 5 – Update or Delete Recalls
We’re sure you know this already (and it was highlighted in Blog 1) but marking off the recall is definitely the most important safety tip so it had to be on this list. If the recall is not removed when the patient returns, your practice recall system will be ineffective and by that we mean increased clinical risk, increased medico-legal risk, complete waste of staff time, waste of doctors/practice money and potentially alarming patients unnecessarily and causing deterioration in reputation and relationships. There are good reasons why doctors struggle to mark recalls as performed but there are equally good reasons why it is absolutely essential. Successful practices build good relationships with patients so they choose to return to them and maintaining a safe, efficient recall and reminder system is vital for effective patient relationships.
Knowing your software is vital to any successful practice Recall and Reminder System. Let us help you with your ‘Quality Improvement’ – contact us today to organise a workshop or online session.
Free Resources:
“Recalls & Reminders using MedicalDirector Clinical” – Katrina Otto’s PowerPoint presentation from (2 hour) Recalls workshop – June 2018.
Cleaning up recalls -summary sheet
Sample recall protocol/flowchart
Practice Success Story: 5 Star Medical (Quality Improvement PDSA)
Train IT Medical Practice Management Free Resources and Helpful Links
MedicalDirector.com official website & learning resources
With best wishes from the Train IT Medical trainers